Disc Herniations: Understanding the Condition and Your Treatment Options
Disc herniations are a leading cause of back pain, neck pain, and nerve-related symptoms in the spine. When the soft inner core of a spinal disc pushes through its outer layer, it can press on nearby spinal nerve roots or the spinal cord, leading to pain, numbness, or muscle weakness. This condition can affect the cervical, thoracic, or lumbar spine and may result from aging, injury, or disc degeneration.
At Verispine Joint Centers, we provide clear diagnosis and evidence-based treatment options to relieve pain, restore function, and help patients return to daily life.
Anatomy Refresher: Understanding the Spine
The spine supports the body, protects the spinal cord, and enables movement. Understanding its structure helps explain how disc herniations develop and why they cause symptoms like back pain, leg pain, and nerve compression.
Spinal Regions and Their Function
The spinal column is divided into three main sections: the cervical spine, thoracic spine, and lumbar spine.
- The cervical spine consists of seven vertebrae in the neck. It supports the head and allows for movement.
- The thoracic spine includes twelve vertebrae in the upper back, attaching to the ribs.
- The lumbar spine contains five vertebrae in the lower back. It bears the most body weight and is the most common site for a disc herniation.
Intervertebral Discs and Their Role
Between each vertebra lies an intervertebral disc, which acts as a cushion and shock absorber. Each disc contains a tough outer ring (annulus fibrosus) and a gel-like center (nucleus pulposus). A disc herniation occurs when the inner material pushes through the outer ring, often into the spinal canal, leading to nerve root compression.
Spinal Cord and Nerve Roots
The spinal cord runs through the spinal canal and branches into spinal nerve roots at each vertebral level. These nerves control muscle strength, reflexes, and sensation. When a herniated nucleus pulposus presses on a nerve root, it can cause sharp pain, muscle weakness, and pain numbness or weakness in the limbs.
Disc Herniation and the Lumbar Spine
Most disc herniations occur in the lumbar spine. This area handles heavy loads and allows for bending and lifting. Lumbar disc herniation often causes leg pain through irritation of the sciatic nerve. This is why the straight leg raise test is used during the physical exam to check for nerve compression.
Spinal Imaging for Diagnosis
To visualize herniated discs, doctors use MRI scans or CT scans. These images show disc material pressing against the spinal cord or surrounding cerebrospinal fluid spaces. Imaging helps confirm a herniated lumbar disk, cervical disc herniation, or other forms of intervertebral disc diseases.
Understanding this anatomy allows for accurate diagnosis and helps guide effective treatment for disc herniations.
What Causes a Disc Herniation?
A herniated disc occurs when the soft inner material of an intervertebral disc pushes through its outer layer, often resulting in back pain, leg pain, or nerve compression. Several factors increase the risk of this condition.
Disc Degeneration and Aging
The most common cause of disc herniations is disc degeneration. Over time, the discs lose water content and become less flexible. This makes them more prone to tearing or rupturing with minor strain. Intervertebral disc diseases often develop with age, leading to chronic low back pain or cervical disc herniation.
Repetitive Stress and Poor Body Mechanics
Frequent bending, twisting, and heavy lifting can place mechanical stress on the spinal column. Poor posture and improper lifting techniques increase pressure on the lumbar spine, raising the risk for a disc herniation. Jobs or activities involving repetitive motion are common risk factors.
Sudden Injury or Trauma
Direct trauma, such as a fall or car accident, can cause a ruptured disk or slipped disk. When force is applied to the spinal bones, the disc material may shift or tear, leading to immediate nerve root compression and severe pain.
Genetic and Structural Factors
Some individuals are born with weaker discs or a narrower spinal canal, making them more likely to suffer from disc herniations. A family history of disc disease may also increase the chance of early disc degeneration and spinal cord compression.
Lifestyle and Health Habits
Smoking, obesity, and lack of physical activity can weaken spinal structures and accelerate disc wear. Extra weight places additional load on the lumbar disc, while poor circulation reduces the disc’s ability to repair itself. These conditions raise the chance that disc herniations occur under normal pressure.
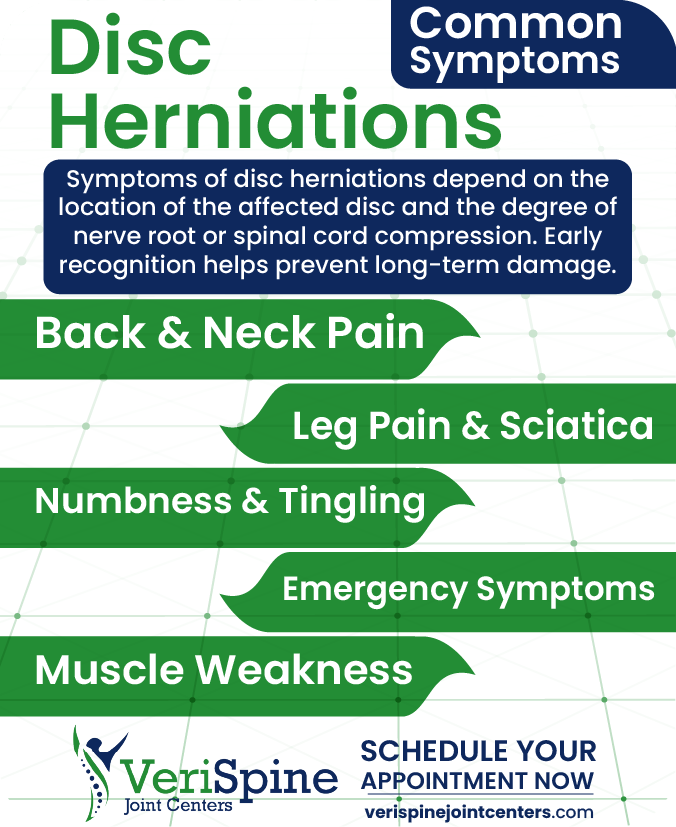
Symptoms of Disc Herniations
Symptoms of disc herniations depend on the location of the affected disc and the degree of nerve root or spinal cord compression. Early recognition helps prevent long-term damage.
Back Pain and Neck Pain
A herniated lumbar disc often causes back pain that may radiate into the hips or legs. Pain may worsen with movement, coughing, or sitting. A cervical disc herniation causes neck pain that may spread to the shoulders or arms. In both cases, the pain is often described as sharp or burning.
Leg Pain and Sciatica
When a disc herniation presses on a nerve root in the lumbar spine, it can lead to leg pain, commonly known as sciatica. This pain travels from the lower back down the buttock and into the leg. The straight leg raise test may reproduce this pain during a physical examination. Sciatica is often a sign of herniated lumbar disk or lumbar disk herniation.
Numbness and Tingling
Compression of spinal nerve roots can cause pain numbness or weakness in the arms or legs, depending on the disc’s location. A herniated disk in the cervical spine may affect the hands and fingers. A herniation in the lumbar region often causes numbness in the foot or lower leg.
Muscle Weakness
A compressed nerve root can interfere with signals between the brain and muscles. This may lead to muscle weakness, reduced grip strength, or difficulty lifting the foot. Over time, this can affect balance and daily movement.
Severe or Emergency Symptoms
In rare cases, disc herniations cause cauda equina syndrome, a serious condition involving loss of bladder or bowel control, numbness in the saddle region, and sudden muscle weakness. This requires immediate medical attention to prevent permanent damage.
Diagnosis: How Disc Herniations Are Confirmed
Accurate diagnosis of a disc herniation involves reviewing symptoms, performing a physical examination, and using spinal imaging to confirm the affected area and level of nerve compression.
Medical History and Symptom Review
The process begins with a detailed medical history. Patients describe the location, intensity, and duration of back pain, neck pain, leg pain, or other symptoms. Specific details about muscle weakness, numbness, or bowel control issues help guide further testing. Risk factors such as prior injuries, repetitive strain, or disc degeneration are also reviewed.
Physical Examination and Nerve Testing
A physical examination checks reflexes, muscle strength, and sensory changes. The provider may perform the straight leg raise test to assess nerve irritation in the lumbar spine. Weakness in grip or arm movement may suggest a cervical spine issue. These findings help identify which spinal nerve roots may be affected by a herniated disk.
Spinal Imaging Techniques
To confirm a diagnosis, spinal imaging is used. An MRI scan is the most common tool to visualize herniated discs, showing the soft tissues, intervertebral discs, and any spinal cord compression. A CT scan may be used when MRI is not an option or when bone detail is needed. These scans detect the location of the disc herniation, size of the extrusion, and impact on surrounding structures, including cerebrospinal fluid spaces.
Differentiating from Other Conditions
Symptoms of disc herniations can overlap with other spinal disorders. The diagnosis must rule out muscle strains, spinal tumors, infections, or fractures. Accurate diagnosis ensures the right course of treatment, whether that involves nonsurgical treatment, epidural injections, or surgical intervention.
Conservative Treatment Options
Most disc herniations improve with non-invasive care. Conservative treatment helps reduce inflammation, relieve pain, and restore function without surgery.
Initial Treatment Approach
The first step often includes bed rest for a short period to reduce stress on the spinal cord and nerve roots. This may be followed by gradual return to activity. Pain medication and muscle relaxers are commonly used to manage severe pain and muscle spasms. These help patients move more comfortably and begin further care.
Physical Therapy and Exercise
Physical therapy plays a key role in managing herniated discs. Stretching and strengthening exercises improve muscle strength, support the spinal column, and promote healing. Therapy may include guided movement, posture training, and core stabilization to reduce pressure on the herniated disk.
Epidural Injections for Pain Relief
In cases of persistent back pain or leg pain, doctors may recommend epidural steroid injections or epidural corticosteroid injections. These are delivered near the affected spinal nerve roots to reduce inflammation. In many cases, injections provide enough relief to delay or avoid surgical treatment.
Spinal Manipulation and Other Methods
For some patients, spinal manipulation may help reduce pressure in the spine and ease discomfort. This must be done by trained professionals to avoid further injury. Heat therapy, cold packs, and electrical stimulation are also used as part of a broader nonsurgical treatment plan.
Monitoring and Reassessment
Conservative care often lasts several weeks. During this time, symptoms are monitored. If there is no improvement or if muscle weakness and nerve compression worsen, further spinal imaging or surgical intervention may be considered.
When Surgery Becomes Necessary
Surgery for disc herniations is considered when conservative treatment fails or when symptoms become severe. The goal is to relieve nerve compression and restore function.
Signs Conservative Treatment Has Failed
If chronic back pain, leg pain, or neck pain continues after several weeks of nonsurgical treatment, surgery may be needed. Persistent muscle weakness, limited mobility, or loss of sensation suggest that the herniated disc is pressing on a nerve root or the spinal cord. When pain disrupts daily life or sleep despite therapy and pain medication, surgical options are evaluated.
Emergency Symptoms Requiring Immediate Surgery
Certain symptoms demand urgent surgical intervention. These include sudden loss of bowel control, severe muscle weakness, or cauda equina syndrome. These problems can result from extreme spinal cord compression or a large herniated lumbar disk and must be addressed quickly to prevent permanent damage.
Common Surgical Procedures
The type of surgery depends on the location and severity of the disc herniation. A microdiscectomy is often used to remove the portion of the disc material pressing on a spinal nerve root. In other cases, a laminectomy or spinal fusion may be needed to stabilize the spinal column and relieve pressure. Surgery is most often performed on the lumbar spine or cervical spine.
What to Expect After Surgery
After surgery, most patients experience reduced pain and improved function. Recovery includes a period of rest followed by physical therapy to regain muscle strength and flexibility. Post-surgical care helps prevent future disc herniations and supports long-term spinal health.
Life After a Herniated Disc
Recovery from a disc herniation continues after symptoms improve. Long-term habits play a key role in protecting the spine and preventing future problems.
Rehabilitation and Strength Building
Physical therapy remains important after initial recovery. Targeted exercises restore muscle strength, improve flexibility, and support the spinal column. Strong muscles help reduce stress on the intervertebral discs and improve posture. Patients may also learn movement patterns that lower the risk of another disk herniation.
Preventing Recurrence
Avoiding heavy lifting, maintaining a healthy weight, and practicing proper body mechanics are key to preventing a new herniated disk. Ongoing attention to posture during sitting, standing, and sleeping reduces pressure on the lumbar spine and cervical spine. Stopping smoking and staying active also support disc health by improving circulation and slowing disc degeneration.
Managing Chronic Symptoms
Some patients continue to experience chronic low back pain or occasional leg pain even after treatment. In these cases, nonsurgical treatment such as epidural injections, mild pain medication, or periodic therapy may help control symptoms. Monitoring by a spine specialist ensures early action if new signs of nerve compression appear.
Long-Term Outcomes
Most people with a history of disc herniations return to normal activities with minimal restriction. With consistent care and attention to spinal health, the risk of another herniated nucleus pulposus can be reduced. Regular check-ins and imaging may be advised if symptoms return or if there are signs of further intervertebral disc issues.
Why Choose Verispine Joint Centers
Verispine Joint Centers provides specialized care for patients with disc herniations and related spinal conditions. Each patient receives focused treatment based on their symptoms and needs.
Expertise in Disc Herniations
The team at Verispine has experience treating a full range of intervertebral disc diseases, including herniated lumbar discs, cervical disc herniation, and disc degeneration. Providers understand the impact of spinal nerve root compression and use clear diagnostic methods to confirm the cause of back pain, neck pain, or leg pain.
Comprehensive Diagnostic Tools
Verispine uses advanced spinal imaging such as MRI scans and CT scans to visualize disc herniations and assess pressure on the spinal cord or nerve roots. A complete physical examination and medical history help guide decisions. Tests like the straight leg raise identify the affected nerve root and clarify the level of involvement.
Focused Nonsurgical and Surgical Options
Treatment plans begin with conservative treatment when possible. This includes physical therapy, epidural steroid injections, and pain medication. When needed, Verispine also offers surgical treatment options including microdiscectomy and spinal decompression. Each patient is monitored to ensure their care supports full recovery.
Multiple Locations for Accessible Care
Verispine Joint Centers has clinics in Stockbridge, Hapeville, Roswell, Decatur, and Lawrenceville. This allows patients to access care for disc herniations, nerve compression, and chronic back pain without delay.
Patient-Focused Approach
Care at Verispine focuses on restoring mobility, reducing pain, and preventing future injury. Whether managing a recent disc herniation or long-term chronic low back pain, the team provides guidance and support through every stage of treatment and recovery.
Frequently Asked Questions About Disc Herniations
What are the early signs of a disc herniation?
Early signs of a disc herniation include lower back pain, sharp leg pain, and numbness or tingling in the foot. These symptoms often result from spinal nerve root compression in the lumbar spine. Muscle weakness and pain with movement may also appear.
How do doctors diagnose a disc herniation in the spine?
Doctors diagnose a disc herniation using a medical history, physical examination, and spinal imaging. MRI scans are most useful to visualize disc herniations and compressed nerve roots. CT scans may help when bone detail is needed.
Can a disc herniation heal without surgery or epidural injections?
Yes, many disc herniations improve without surgery or injections. Physical therapy, rest, and pain medication often relieve symptoms. Epidural steroid injections may be added if pain persists after several weeks of nonsurgical treatment.
What causes disc herniations in the lower back or neck?
Disc herniations in the lower back or neck are usually caused by disc degeneration, poor posture, or injury. Age, repetitive strain, and mechanical compression increase the risk. The disc material pushes into the spinal canal and may compress nerve roots.
How long does it take to recover from a disc herniation?
Most people recover from a disc herniation within six to twelve weeks using conservative treatment. Surgical recovery for disc herniations may take longer but often leads to faster pain relief. Long-term recovery focuses on strengthening and preventing future disc problems.
Take the Next Step with Verispine Joint Centers
Disc herniations can cause lasting pain and limit your daily activity, but effective treatment is available. Whether you are dealing with back pain, leg pain, or nerve symptoms caused by a disc herniation, early evaluation can prevent long-term damage.
Our team at Verispine Joint Centers specializes in diagnosing and treating spinal conditions with a focus on clear solutions and proven results. If you are ready to relieve pain and restore function, contact us today to schedule your consultation!