Osteoarthritis: Understanding the Most Common Cause of Joint Pain
Osteoarthritis is the most common form of joint disease, affecting millions of people living with daily pain, stiffness, and limited mobility. This degenerative condition occurs when the cartilage that cushions the joints wears down over time, leading to joint damage, swelling, and reduced function.
Whether caused by aging, past joint injury, or excess stress on weight-bearing joints, osteoarthritis can significantly impact your quality of life. At Verispine Joint Centers, our osteoarthritis specialists provide personalized treatment plans designed to manage symptoms, reduce pain, and improve joint function. Our comprehensive treatment options include non-surgical therapies, minimally invasive procedures, and ongoing care strategies that target the specific needs of each patient. By combining advanced diagnostic techniques with expert specialists, we guide patients through the most effective treatment approaches for long-term joint health.
From initial evaluation to ongoing management, our team ensures that every patient receives tailored treatment for osteoarthritis, helping restore mobility, relieve discomfort, and maintain independence. With Verispine Joint Centers as your trusted guide, you can explore the full range of available treatment options under the care of experienced specialists dedicated to your recovery.
What Is Osteoarthritis?
Osteoarthritis is the most common form of joint disease. It develops when joint cartilage breaks down, causing pain, stiffness, and limited movement in the affected joints. This condition can impact people of all ages, but it is more common in older adults and those with a history of joint injury.
Degenerative Joint Disease
Osteoarthritis is a type of degenerative joint disease. It causes the cartilage in joints to wear away over time. Cartilage is the slippery tissue that covers the ends of bones in a healthy joint. When this tissue wears down, bones may rub against each other, leading to joint pain and swelling.
Joint Cartilage and Joint Lining Breakdown
As the disease progresses, the joint lining becomes inflamed and the joint space narrows. This can lead to the formation of bone spurs and further joint damage. Over time, the breakdown of cartilage and other joint tissues reduces the joint’s ability to move smoothly.
Primary and Secondary Osteoarthritis
There are two main types of osteoarthritis. Primary osteoarthritis develops with age and is linked to general wear and tear. Secondary osteoarthritis happens due to a previous joint injury, joint instability, or an underlying condition like rheumatoid arthritis or other musculoskeletal and skin diseases.
Joints Commonly Affected
This condition affects weight-bearing joints like the hips, knees, and spine. It can also impact smaller joints such as finger joints and those in the hands or feet. Hip osteoarthritis and ankle osteoarthritis are common in people with long-term joint stress or injury.
Disease Progression
Osteoarthritis increases gradually. Early stages may cause mild joint stiffness. As the disease worsens, symptoms become more severe. The joint capsule, connective tissues, and underlying bone may all be affected, leading to chronic pain and reduced quality of life.
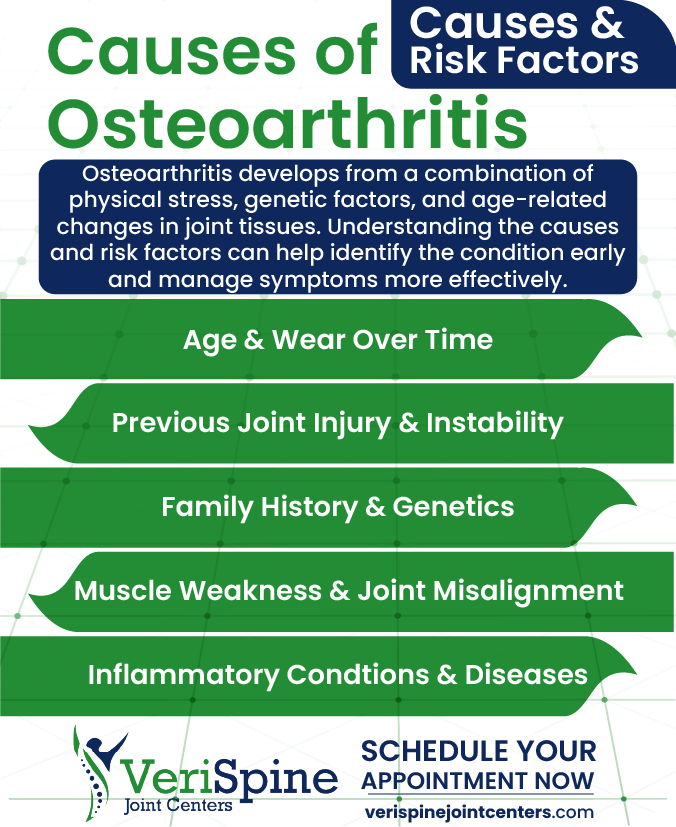
Causes and Risk Factors
Osteoarthritis develops from a combination of physical stress, genetic predisposition, and age-related changes in joint tissues. Understanding the causes and risk factors for osteoarthritis can help patients recognize early signs, seek timely evaluation, and begin appropriate treatment to manage symptoms effectively.
Age and Wear Over Time
Age is the most common risk factor for osteoarthritis. As people age, the cartilage in their joints naturally wears down. This wear reduces the joint’s ability to absorb shock and support smooth movement. Older adults are more likely to develop osteoarthritis due to this gradual degeneration.
Previous Joint Injury and Instability
A history of joint injury increases the chance of developing osteoarthritis. Damage from sports, accidents, or surgery can weaken the joint structure. Joint instability also puts stress on the cartilage and joint capsule, speeding up the breakdown process.
Obesity and Weight-Bearing Stress
Excess body weight places pressure on weight-bearing joints like the knees, hips, and lower back. This added stress can lead to joint damage and inflammation. Obesity also increases the production of chemicals that may cause joint tissue breakdown.
Family History and Genetics
A family history of osteoarthritis can increase a person’s risk. Genetic factors may affect how cartilage forms or how the body responds to joint stress. People with inherited joint traits are more likely to experience early cartilage wear and joint pain.
Muscle Weakness and Joint Misalignment
Weak muscles around a joint can affect joint stability. Poor alignment of the bones in a joint can also cause uneven wear on the cartilage. Both factors contribute to the development and progression of osteoarthritis.
Other Conditions and Inflammatory Diseases
People with conditions like rheumatoid arthritis or other musculoskeletal and skin diseases may be at higher risk for secondary osteoarthritis. Chronic inflammation and damage to connective tissues can speed up joint degeneration.
Symptoms of Osteoarthritis
Osteoarthritis symptoms often develop gradually and worsen over time, making early recognition critical. Identifying these signs promptly allows patients to seek evaluation from osteoarthritis specialists and begin effective treatment plans that reduce pain, protect joint function, and improve mobility. At Verispine Joint Centers, our team helps patients understand the progression of osteoarthritis and guides them through personalized treatment strategies designed to manage symptoms and prevent further joint damage. Early intervention with the right specialists can slow disease progression, reduce discomfort, and support long-term joint health.
Joint Pain and Stiffness
Pain is the most common symptom of osteoarthritis. It often starts as a dull ache in the affected joints, especially after activity. Joint stiffness usually occurs in the morning or after long periods of inactivity. Movement may relieve stiffness temporarily, but pain can return with continued use.
Limited Joint Movement
As the disease progresses, joint movement becomes more difficult. The joint may feel tight, and full range of motion may be lost. Simple tasks such as bending, gripping, or walking can become harder to perform. Reduced mobility often leads to muscle weakness around the joint.
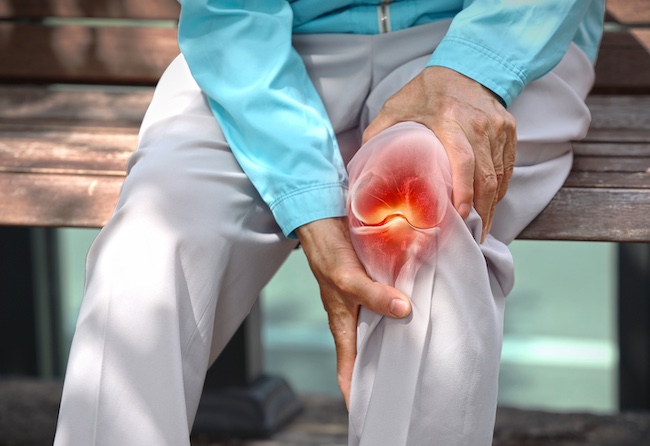
Swelling and Tenderness
Osteoarthritis can cause joint swelling due to inflammation and fluid buildup. The affected joints may feel tender when touched. In some cases, the joint may appear larger due to bone spurs or joint space changes.
Bone Spurs and Joint Instability
Bone spurs are small bony growths that form around the joint as cartilage wears away. They can cause irritation and limit motion. In severe osteoarthritis, the joint may feel unstable or give out during movement. This is more common in weight-bearing joints such as the hip or knee.
Commonly Affected Joints
Osteoarthritis commonly affects the knees, hips, spine, hands, and finger joints. Hip osteoarthritis may cause pain in the groin, thigh, or buttock. Ankle osteoarthritis often results from previous joint injury and can make walking painful and unsteady.
Worsening Symptoms
Symptoms of osteoarthritis often become worse over time. Pain and stiffness may increase, especially with weather changes or extended activity. Severe symptoms can interfere with sleep, work, and overall quality of life. Chronic pain may signal advanced joint damage and reduced joint space.
How Osteoarthritis Is Diagnosed
Diagnosis of osteoarthritis begins with a comprehensive evaluation by trained osteoarthritis specialists who can guide patients toward the most effective treatment options. Early and accurate diagnosis is essential for managing symptoms, reducing pain, and slowing joint damage. At Verispine Joint Centers, our team of specialists works closely with patients to assess joint function, review medical history, and design a personalized treatment plan that addresses the specific severity and progression of osteoarthritis. Prompt consultation with our osteoarthritis specialists ensures patients receive the right treatment early, improving mobility, quality of life, and long-term joint health.
Medical History and Symptoms
The diagnostic process begins with a detailed medical history. The provider will ask about symptoms such as joint pain, stiffness, swelling, and changes in movement. They will also consider factors like age, previous joint injury, and family history of joint disease.
Physical Examination
A physical examination helps assess joint function and detect signs of osteoarthritis. The provider will check for tenderness, swelling, limited range of motion, and joint instability. They may also evaluate muscle strength and alignment of the affected joints.
Imaging and Diagnostic Tests
X-rays are commonly used to confirm osteoarthritis. They can show joint space narrowing, bone spurs, and damage to joint cartilage. In some cases, MRI scans provide a more detailed view of joint tissues, including the joint capsule and surrounding structures.
Differentiating from Other Conditions
Osteoarthritis must be distinguished from other forms of arthritis, such as rheumatoid arthritis. Blood tests may be ordered to rule out inflammatory or autoimmune diseases. This helps ensure the correct treatment plan is selected.
Monitoring Disease Progression
Once osteoarthritis is diagnosed, providers track symptoms and joint changes over time. Monitoring helps guide treatment decisions and determine when to adjust care to improve pain and function.
Treatment Options for Osteoarthritis
Osteoarthritis treatment focuses on reducing pain, improving joint function, and slowing disease progression. At Verispine Joint Centers, our osteoarthritis specialists develop personalized treatment plans that combine medical, non-medical, and interventional approaches. The right treatment can include lifestyle modifications, physical therapy, medications, joint injections, and, when necessary, surgical options. Our team guides patients through every step of their osteoarthritis treatment, ensuring each individual receives the most effective interventions to manage symptoms, maintain mobility, and improve quality of life.
Lifestyle Changes
Weight management helps reduce stress on weight-bearing joints such as the knees and hips. Regular low-impact exercise can improve joint movement and muscle strength. A physical therapist may develop a program to relieve stiffness and support joint stability.
Medications for Pain Relief
Pain medications are often used to manage osteoarthritis symptoms. These may include acetaminophen, non-steroidal anti-inflammatory drugs, or topical treatments. In more advanced cases, prescription drugs or disease modifying drugs may be considered.
Joint Injections
Joint injections can relieve pain and decrease swelling in affected joints. Corticosteroid injections reduce inflammation, while hyaluronic acid injections may help lubricate the joint space. These options can provide temporary relief, especially for hip or knee osteoarthritis.
Physical and Occupational Therapy
A physical therapist can teach exercises that reduce pain and improve range of motion. An occupational therapist may help adapt daily activities to avoid putting stress on painful joints. Therapy supports better function and reduces the risk of further joint damage.
Surgical Options
When other treatments fail, joint surgery may be needed. Joint replacement surgery is common for severe osteoarthritis in the hip or knee. It involves removing the damaged joint surface and replacing it with artificial components to restore function.
Complementary Therapies and Clinical Trials
Some people with osteoarthritis explore complementary medicine such as acupuncture or supplements. Clinical trials may also offer access to new treatment options that are being studied for safety and effectiveness.
How Verispine Joint Centers Can Help
At Verispine Joint Centers, our osteoarthritis specialists guide patients through personalized treatment plans designed to reduce pain, restore movement, and slow disease progression. From the initial consultation to ongoing management, our team ensures each patient understands their treatment options and receives the most appropriate interventions. Whether through non-surgical care, interventional procedures, or long-term management strategies, our specialists provide expert oversight at every stage of osteoarthritis treatment, helping patients regain mobility and improve quality of life.
Comprehensive Evaluation
Each patient receives a full assessment that includes a physical exam, imaging, and review of symptoms. Providers look for signs of joint damage, joint space narrowing, and joint instability to understand the severity and location of the condition.
Non-Surgical Treatment Plans
Verispine prioritizes non-surgical options when possible. These may include physical therapy, joint injections, and pain medications. The goal is to relieve stiffness, reduce pain, and improve function without immediate surgery.
Advanced Interventional Care
For patients with severe osteoarthritis or limited response to conservative care, Verispine offers advanced solutions. This includes minimally invasive procedures and joint replacement planning. Hip osteoarthritis and other weight-bearing joint conditions are evaluated for appropriate surgical intervention if needed.
Patient Education and Support
Patients are given clear information about their condition and treatment options. The team explains how to manage symptoms and prevent further joint damage. Education supports long-term improvement in quality of life and joint health.
Multiple Locations for Easy Access
Verispine Joint Centers operates in several locations, making it easier for patients to access expert care. Whether managing early osteoarthritis symptoms or seeking advanced treatment, patients receive care that focuses on their needs.
When to Seek Help for Osteoarthritis
Recognizing when to seek professional treatment for osteoarthritis is essential to prevent further joint damage, reduce pain, and restore mobility. Verispine Joint Centers’ experienced specialists guide patients through early and advanced treatment options to preserve joint health and improve quality of life.
Persistent Pain and Stiffness
If joint pain or stiffness persists for weeks or disrupts daily activities, it’s time to consult osteoarthritis specialists. Early treatment can relieve discomfort, reduce inflammation, and slow the progression of joint damage, helping you maintain independence and mobility.
Limited Joint Movement
Difficulty bending or moving a joint, or a noticeable loss of flexibility in the knees, hips, hands, or spine, signals the need for professional treatment. Our specialists design personalized treatment plans that strengthen muscles, improve joint function, and restore range of motion.
Joint Instability or Weakness
Joints that feel unstable, weak, or prone to giving out during movement require evaluation by osteoarthritis specialists. Targeted treatment can stabilize the joint, reduce the risk of injury, and support safe daily activities.
Swelling, Warmth, or Deformity
Swelling, warmth, or visible changes in joint structure may indicate advanced osteoarthritis. Verispine specialists provide advanced treatment options, including joint injections and non-surgical interventions, to reduce pain, improve function, and prevent further joint damage.
Ineffective Home Care
If rest, ice, over-the-counter medications, and activity adjustments no longer manage symptoms effectively, it’s time to seek professional treatment. Our specialists create comprehensive treatment plans that include physical therapy, injections, and minimally invasive procedures tailored to your condition and lifestyle.
Frequently Asked Questions About Osteoarthritis
Osteoarthritis affects millions and is the most common form of joint disease. If you’re experiencing joint pain, stiffness, or reduced mobility, these questions and answers can help you better understand the condition, its causes, and how it can be treated.
What is the difference between osteoarthritis and rheumatoid arthritis?
This condition is a degenerative joint disease that develops when cartilage and surrounding joint tissues wear down over time, often due to aging, prior injury, or repetitive stress. In contrast, rheumatoid arthritis is an autoimmune disorder where the immune system attacks the joint lining, leading to inflammation and damage. While both cause pain and stiffness, degenerative arthritis is more likely to affect weight-bearing joints such as the knees and hips.
How do I know if I have it or just joint pain from aging?
Persistent pain, stiffness after rest, swelling, limited movement, or a grinding sensation during motion may point to more than general aging. These symptoms often worsen with time and can interfere with daily tasks. A physical exam and imaging can determine whether joint pain is age-related or a sign of a chronic joint disease.
What are the best treatment options for joint pain relief?
Effective treatments include weight loss, regular low-impact exercise, physical therapy, medications, and joint injections. In advanced cases, joint replacement surgery may be needed. Therapies like disease modifying drugs and anti-inflammatory treatments can also help manage symptoms and slow progression.
What joints are most commonly affected?
The knees, hips, and spine are most frequently impacted, especially in those who carry excess weight or have a history of injury. Smaller joints, including those in the fingers, thumbs, and ankles, can also be involved. Wear and tear, joint space narrowing, and the development of bone spurs often occur in these areas.
Can the condition get worse if left untreated?
Yes, it often progresses when not addressed. What starts as mild discomfort and stiffness can advance to chronic pain, joint instability, and restricted movement. Early intervention helps preserve function, ease symptoms, and slow further damage.
Take Control of Osteoarthritis with Expert Care
Living with osteoarthritis can limit your movement, disrupt daily life, and cause ongoing joint pain. Early diagnosis and a comprehensive treatment plan can reduce symptoms, protect your joints from further damage, and guide you toward lasting relief.
Our team at Verispine Joint Centers is here to help you manage osteoarthritis with expert care, personalized treatment options, and a clear focus on improving joint function and reducing discomfort. We develop tailored treatment strategies that combine medical, physical, and interventional approaches to meet your individual needs.
If you’re ready to take the next step in your osteoarthritis treatment, contact us today to schedule your consultation and begin a plan designed to restore mobility, reduce pain, and improve quality of life 678-782-7999