Post-Laminectomy Syndrome | Understanding the Challenges of Chronic Pain After Spine Surgery
If you’re experiencing persistent back or leg pain after spinal surgery, you’re not alone—and there is hope. Post-laminectomy syndrome (also called failed back surgery syndrome) affects up to 40% of patients who undergo spine surgery. At Verispine Joint Centers in Metro Atlanta, our specialized team has successfully treated hundreds of patients struggling with chronic pain after laminectomy, fusion, or discectomy procedures.
Whether your pain is caused by scar tissue, recurrent disc herniation, or nerve damage, we offer advanced, evidence-based treatments that can provide significant relief without additional surgery.
Don’t suffer in silence. Call 678-782-7999 or schedule online today. Same-week appointments available at all Metro Atlanta locations.
Post-Laminectomy Syndrome Treatment in Atlanta | Failed Back Surgery Pain Relief
Post-laminectomy syndrome is a condition where patients continue to experience back or leg pain after undergoing spinal surgery. It is also referred to as failed back surgery syndrome and often arises after procedures such as lumbar laminectomy, lumbar discectomy, or spinal fusion.
Understanding Failed Back Surgery Syndrome
Post-laminectomy syndrome refers to persistent or recurring pain following spinal surgery. The pain may occur in the lower back, legs, or neck. Although spine surgeries are designed to alleviate pressure on the spinal nerves or stabilize the spine, not all patients experience relief, and some may continue to suffer from ongoing discomfort.
What Causes Chronic Pain After Spine Surgery?
Post-laminectomy syndrome can result from several factors. A common cause is the formation of scar tissue, also known as epidural fibrosis, around the nerve roots. Recurrent lumbar disc herniation, spinal instability, or incomplete removal of a disc can also contribute to ongoing pain. After lumbar fusion surgery, patients may develop new issues like adjacent segment degeneration or spinal stenosis. Nerve injury during the surgery is another potential cause of persistent pain.
Laminectomy, Fusion & Discectomy Complications
Procedures most frequently associated with post-laminectomy syndrome include lumbar laminectomy, spinal fusion, and lumbar discectomy. These surgeries are often performed to treat conditions like herniated discs, spinal stenosis, and chronic low back pain. In some cases, the surgery may not fully address the pain generator, or new sources of pain may arise.
Recognizing Post-Surgical Pain Symptoms
Symptoms of post-laminectomy syndrome often include chronic nerve pain, stabbing pain, or neuropathic pain in the back or legs. The pain may persist or recur weeks, months, or even years after the surgery. Some patients also report sacroiliac joint pain or pain with no clear origin. These symptoms can significantly affect mobility and overall quality of life.
Related Chronic Spine Pain Conditions
Post-laminectomy syndrome shares similarities with other chronic pain syndromes, such as spinal nerve root irritation, inflammatory spinal pain, and recurrent disc herniation. It is a leading cause of long-term low back pain disability, as well as increased pain intensity that affects daily activities.
Experiencing these symptoms? Get an expert evaluation. Early intervention leads to better outcomes. Call 678-782-7999.
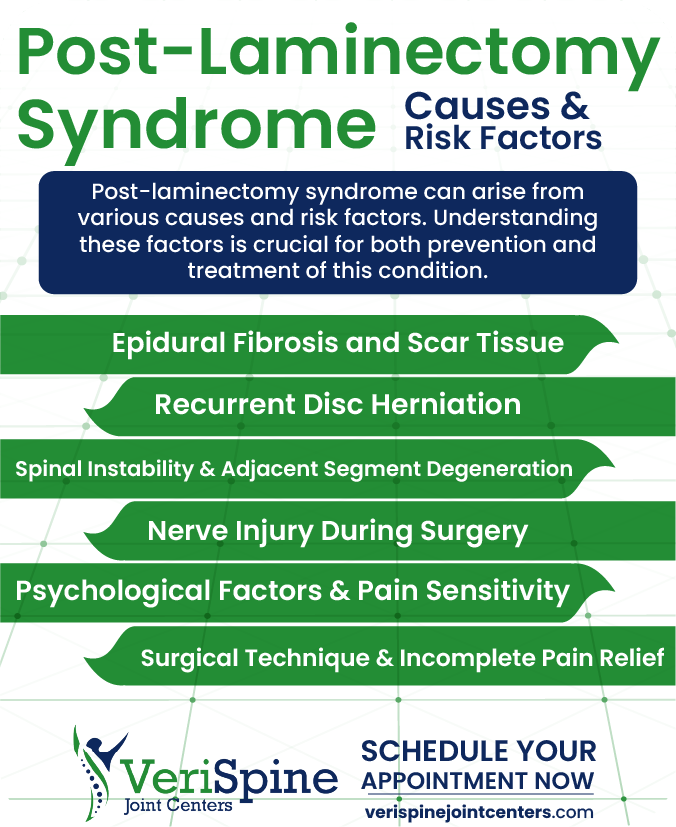
Causes of Chronic Pain After Spine Surgery
Post-laminectomy syndrome can arise from various causes and risk factors. Understanding these factors is crucial for both prevention and treatment of this condition.
Scar Tissue Formation Around Nerve Roots (Epidural Fibrosis)
One of the primary causes of post-laminectomy syndrome is epidural fibrosis, the formation of scar tissue around the nerve roots. After spinal surgery, this scar tissue can compress or irritate the nerves, leading to chronic pain. This condition is often seen in patients who have undergone lumbar laminectomy or lumbar discectomy.
Recurrent Herniated Disc After Surgery
Recurrent lumbar disc herniation is another common cause of persistent pain after surgery. Even after a disc is removed or repaired, the herniation may return, leading to new or worsened spinal pain. This is especially common in patients who undergo laminectomy procedures for herniated discs.
Spinal Instability and Adjacent Segment Disease
After spinal fusion surgery or other spine surgeries, the remaining parts of the spine can become unstable. This instability may result in the development of adjacent segment degeneration, where the discs and joints above or below the fusion site begin to deteriorate. This can lead to new sources of pain and discomfort.
Nerve Damage During Spinal Procedures
In some cases, nerve injury during surgery can contribute to post-laminectomy syndrome. Even with careful surgical procedures, nerves in the spinal cord or nerve roots can be damaged, leading to neuropathic pain, weakness, or numbness that persists after recovery.
Pain Sensitivity and Psychological Impact
Psychological factors such as anxiety, depression, or stress can increase pain sensitivity, making patients more susceptible to developing post-laminectomy syndrome. These factors may also contribute to a patient’s perception of pain and how it affects their daily life, potentially worsening the chronic pain experience.
Incomplete Decompression and Surgical Complications
Sometimes, the technique used during spinal surgery does not fully address the pain generator. If the cause of the pain is misidentified or if the surgery is incomplete, patients may continue to experience symptoms. In some cases, the procedure might not fully relieve pressure on the spinal nerves, leading to persistent pain.
Failed Back Surgery Syndrome Symptoms | When to Seek Treatment
Failed back surgery syndrome (FBSS) includes a range of symptoms that can persist or reappear after spinal surgery. Recognizing these signs is key to understanding and managing the condition effectively.
Persistent Lower Back Pain After Surgery
One of the most common symptoms of FBSS is chronic pain. This pain often affects the lower back, but it can also radiate to the legs or neck. Patients may experience constant discomfort, even after recovery from the surgery itself. The pain can be dull, sharp, or stabbing, and it often feels similar to the pain experienced before the surgery.
Burning or Tingling Nerve Pain (Neuropathic Pain)
Neuropathic pain is another hallmark of FBSS. This type of pain is caused by nerve damage or compression and often manifests as a burning or tingling sensation. It can occur in the back, legs, or other parts of the body, depending on which nerves are affected. Neuropathic pain may be accompanied by numbness or weakness in the affected area.
Pain That Returns After Initial Relief
Recurrent pain is a key sign of FBSS. Some patients may experience pain that returns weeks, months, or even years after surgery. This pain is often related to the same area of the spine that was treated. Recurrent pain can be caused by factors like recurrent disc herniation, epidural fibrosis, or spinal instability.
Reduced Range of Motion and Spine Stiffness
Patients with FBSS may notice a decrease in their ability to move freely due to pain or stiffness in the spine. This limitation in mobility can affect daily activities and significantly reduce quality of life. In some cases, patients may find it difficult to bend, lift, or perform other basic movements.
Radiating Leg Pain and Muscle Weakness
In addition to back pain, FBSS often leads to pain and weakness in the legs. This leg pain can be sharp, burning, or aching and may be accompanied by weakness, making it difficult for patients to walk or stand for long periods. Nerve root irritation or damage is a common cause of this symptom.
Unexplained Chronic Pain After Laminectomy
In some cases, patients with FBSS experience pain that cannot be easily traced to a specific source. This pain, often described as pain of unknown origin, can be frustrating for both patients and doctors. It may involve deep, aching sensations in the back or legs, but standard imaging tests may not reveal the underlying cause.
Advanced Diagnostic Testing for Post-Laminectomy Syndrome
Accurately diagnosing post-laminectomy syndrome or failed back surgery syndrome requires a thorough evaluation. This process helps identify the underlying cause of persistent pain and guide appropriate treatment options.
Comprehensive Physical and Neurological Exam
A detailed physical examination is the first step in diagnosing post-laminectomy syndrome. During the exam, the physician will assess the patient’s posture, mobility, and range of motion. The doctor will also test for areas of tenderness or pain and evaluate nerve function, including reflexes and muscle strength. This examination helps identify specific symptoms related to nerve root irritation, spinal instability, or scar tissue formation.
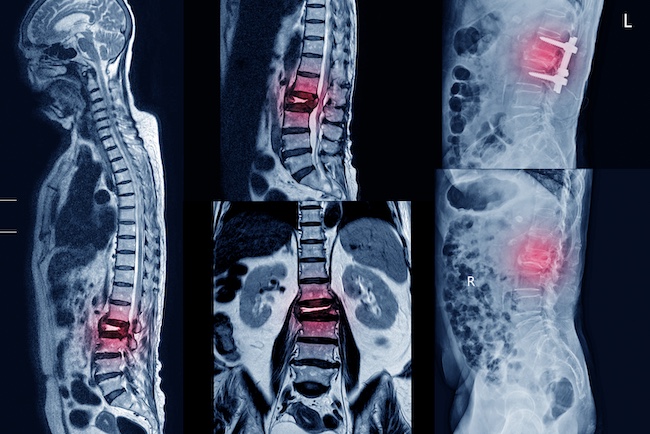
MRI, CT Scan & X-Ray Imaging for Spine Issues
Imaging tests such as MRI, CT scans, or X-rays are crucial for identifying structural issues in the spine. These tests can reveal problems such as recurrent disc herniation, spinal stenosis, or the presence of scar tissue (epidural fibrosis) around the nerve roots. Imaging helps doctors visualize the condition of the lumbar spine, spinal canal, and surrounding structures, which is important for confirming the cause of the pain.
EMG Testing for Nerve Damage Assessment
Electromyography (EMG) is used to evaluate nerve damage or dysfunction. This test measures the electrical activity of muscles and nerves and can help identify nerve injury or compression. It is especially useful in cases where neuropathic pain is present, as it can pinpoint damaged or irritated nerve roots contributing to ongoing pain.
Diagnostic Nerve Blocks and Injection Therapy
Diagnostic injections, such as nerve blocks or epidural steroid injections, are commonly used to identify the source of pain. By injecting a local anesthetic into specific areas of the spine, doctors can determine whether the pain is coming from the spine, nerves, or surrounding tissues. A positive response to the injection can help confirm the pain generator and guide further treatment.
Laboratory Testing to Rule Out Infection
In some cases, blood tests may be conducted to rule out infections or inflammatory conditions that could contribute to persistent pain. These tests can help eliminate other potential causes of pain, such as infections or autoimmune diseases that may mimic symptoms of post-laminectomy syndrome.
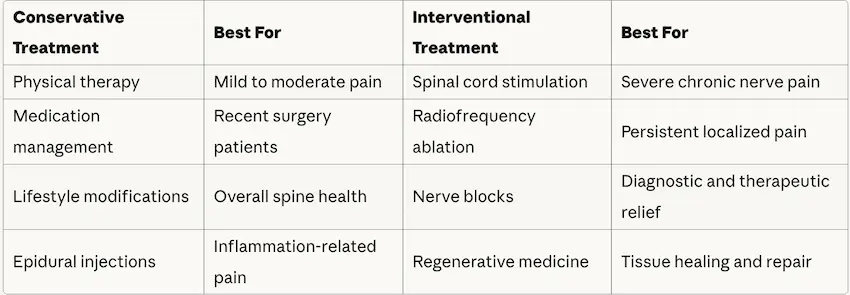
Advanced Pain Relief Therapies | Spinal Cord Stimulation & Interventional Treatments
When conservative treatments are not sufficient, interventional and advanced therapies may provide effective pain relief for patients with post-laminectomy syndrome. These options aim to address the underlying causes of pain with minimally invasive procedures.
Spinal Cord Stimulator Implants for Chronic Pain Relief
Spinal cord stimulation (SCS) is an advanced therapy used to manage chronic nerve pain. This device delivers electrical impulses to the spinal cord to block pain signals before they reach the brain. Spinal cord stimulation is particularly effective for patients with neuropathic pain or those who have not responded to other treatments. It can offer long-term relief and improve function, especially when other methods fail.
Targeted Nerve Block Injections
Nerve blocks are a targeted intervention for pain originating from specific nerve roots. In this procedure, an anesthetic or steroid is injected near the affected nerve to reduce pain and inflammation. Nerve blocks can be diagnostic, helping to identify the pain source, or therapeutic, offering long-term relief for patients with persistent pain following spinal surgery.
Radiofrequency Ablation (RFA) Therapy
Radiofrequency ablation (RFA) is a procedure that uses heat to disrupt the nerve pathways responsible for transmitting pain signals. RFA is typically used when nerve blocks provide temporary relief but the pain returns. This technique can offer significant pain relief for patients with chronic low back pain or leg pain related to nerve root irritation or epidural fibrosis.
Regenerative Medicine: PRP and Stem Cell Therapy
Regenerative medicine therapies, such as platelet-rich plasma (PRP) injections or stem cell therapy, are emerging treatments for post-laminectomy syndrome. These treatments aim to promote healing and tissue regeneration in the affected area. While research is still ongoing, some patients have found relief from pain and inflammation through these cutting-edge therapies.
Revision Surgery for Recurrent Spine Issues
In some cases, repeat surgery may be considered for patients with post-laminectomy syndrome. If new structural issues, such as recurrent disc herniation, spinal instability, or adjacent segment degeneration, are identified, a second surgery may be necessary to address these concerns. However, repeat surgery is typically seen as a last resort after other interventional treatments have failed.
Ready to explore your treatment options? Schedule a consultation at our nearest location. Schedule Now: Call 678-782-7999
Why Choose Verispine for Post-Laminectomy Syndrome Treatment in Georgia?
Verispine Joint Centers offer expert care for patients dealing with post-laminectomy syndrome. Our approach combines advanced treatments with a focus on patient outcomes and quality of life.
Board-Certified Spine Pain Specialists
At Verispine Joint Centers, our team of specialists is highly experienced in diagnosing and treating post-laminectomy syndrome. With a deep understanding of chronic spinal pain, we offer a range of treatments that address the underlying causes of failed back surgery syndrome. Whether your pain is due to epidural fibrosis, recurrent disc herniation, or spinal instability, our experts provide precise, evidence-based solutions.
Multidisciplinary Team Approach to Pain Management
We take a comprehensive approach to managing post-laminectomy syndrome, combining conservative and advanced therapies. Our team includes pain physicians, physical therapists, and spine specialists who work together to create personalized treatment plans. This multidisciplinary approach ensures that each patient receives care tailored to their specific needs, improving both pain relief and functional outcomes.
Minimally Invasive Procedures with Faster Recovery
Verispine Joint Centers prioritize minimally invasive procedures to treat spinal pain. Our advanced techniques, such as spinal cord stimulation, nerve blocks, and radiofrequency ablation, are designed to provide effective pain relief while minimizing recovery time. We aim to offer long-term relief without the need for repeat surgeries, when possible.
Patient-Centered Care and Education
We believe that patient education is a key component of successful treatment. At Verispine, we take the time to explain the causes of your pain, available treatment options, and the expected outcomes. We empower our patients to make informed decisions about their care, ensuring they are involved in the process every step of the way.
5 Convenient Locations Across Metro Atlanta
With multiple locations, including Stockbridge, Hapeville, Roswell, Decatur, and Lawrenceville, Verispine Joint Centers make it easier for patients to access expert spinal care. Our convenient locations allow us to provide timely consultations and treatments, ensuring that help is never far away.
Post-Laminectomy Syndrome FAQs | Patient Questions Answered
Here are answers to some of the most common questions regarding post-laminectomy syndrome, also known as failed back surgery syndrome.
What Is Post-Laminectomy Syndrome and Failed Back Surgery Syndrome?
Post-laminectomy syndrome, or failed back surgery syndrome, refers to ongoing pain following spinal surgery. This can occur after procedures like lumbar laminectomy or spinal fusion. Common causes include scar tissue (epidural fibrosis), recurrent disc herniation, or nerve irritation. While surgery aims to relieve pain, it can sometimes result in persistent or new pain due to complications or incomplete resolution of the underlying issue.
What Are the Main Causes of Pain After Spine Surgery?
Key causes include epidural fibrosis (scar tissue around the nerve roots) and recurrent lumbar disc herniation. Spinal instability, adjacent segment degeneration, or nerve damage during surgery can also lead to persistent pain. Additionally, conditions like spinal stenosis may develop after surgery, contributing to long-term discomfort.
How Is Failed Back Surgery Syndrome Diagnosed?
Diagnosis begins with a physical examination to assess pain levels, mobility, and nerve function. Imaging tests, such as MRI or CT scans, help identify structural issues like herniated discs or scar tissue. Electromyography (EMG) is used to evaluate nerve damage. Diagnostic injections, like nerve blocks, may also pinpoint the pain source.
What Treatment Options Are Available for Post-Laminectomy Syndrome?
Treatments include conservative options like physical therapy, medication, and epidural steroid injections. For more persistent pain, interventional therapies such as spinal cord stimulation (SCS), nerve blocks, or radiofrequency ablation can help. In some cases, repeat surgery may be needed if new problems, like recurrent disc herniation, occur.
Can You Prevent Post-Laminectomy Syndrome?
While prevention of post-laminectomy syndrome isn’t always possible, several steps can reduce the risk. Choosing an experienced surgeon, following post-operative care, and participating in physical therapy can all aid recovery. Maintaining a healthy weight and avoiding strain on the spine can also reduce the likelihood of complications leading to long-term pain.
How long does post-laminectomy syndrome last?
Post-laminectomy syndrome can last from a few months to several years, depending on the underlying cause and treatment approach. Without treatment, symptoms may persist indefinitely. However, patients who receive early intervention typically experience significant improvement within 3-6 months.
Duration factors include:
- Scar tissue formation: May take 3-6 months to stabilize with treatment
- Nerve damage: Can improve over 6-12 months with proper management
- Spinal instability: Often requires ongoing treatment for lasting relief
- Treatment compliance: Consistent therapy leads to faster recovery
Early intervention is critical. Patients who begin conservative treatments like physical therapy and medication management within the first few months after surgery often see faster improvement. For more complex cases requiring interventional therapies such as spinal cord stimulation, symptom relief typically occurs within 3-6 months of treatment initiation.
At Verispine Joint Centers, we create personalized treatment plans designed to provide both short-term relief and long-term pain management. Most of our patients achieve meaningful pain reduction within the first 8-12 weeks of beginning treatment.
Is post-laminectomy syndrome permanent?
No, post-laminectomy syndrome is not necessarily permanent. With appropriate treatment, 60-80% of patients experience significant long-term pain relief. The condition can be effectively managed and often resolved with a comprehensive treatment approach.
Treatment outcomes:
- Conservative therapy: 40-60% of patients achieve lasting relief
- Interventional procedures: 50-70% experience 50% or greater pain reduction
- Spinal cord stimulation: Up to 70% report sustained improvement
- Multimodal approach: Highest success rates with combined therapies
The key is identifying the specific cause of your pain—whether it’s epidural fibrosis, recurrent disc herniation, nerve irritation, or spinal instability—and addressing it with targeted treatment. Prognosis improves dramatically when treatment is individualized and started early.
Treatments that provide lasting relief include:
- Physical therapy and exercise programs
- Medication management protocols
- Epidural steroid injections
- Nerve blocks and radiofrequency ablation
- Spinal cord stimulation for chronic cases
- Regenerative medicine therapies
Our specialists at Verispine Joint Centers work closely with each patient to develop a treatment plan focused on achieving sustained pain relief and preventing symptom recurrence.
What is the success rate of spinal cord stimulation for failed back surgery?
Spinal cord stimulation (SCS) has a 50-70% success rate for failed back surgery syndrome, with patients experiencing at least 50% pain reduction. Many patients report even greater improvement, with some achieving 70-80% pain relief.
Clinical success rates:
- 50-70% of patients achieve ≥50% pain reduction
- 40-50% experience ≥70% pain improvement
- 80-90% report improved quality of life
- 60-70% reduce opioid medication use
- 85% patient satisfaction rate with permanent implants
Success factors that improve outcomes:
- Proper patient selection and screening
- Successful trial period (5-7 days) before permanent implant
- Predominantly neuropathic (nerve) pain pattern
- Treatment within 2-3 years of failed surgery
- Comprehensive pain management approach
The trial phase is crucial—patients test the device for 5-7 days to ensure adequate pain relief before permanent implantation. If the trial succeeds, a permanent stimulator is implanted. Patients typically report improved mobility, reduced medication dependence, and significantly enhanced quality of life.
At Verispine Joint Centers, our pain specialists use the latest SCS technology and follow evidence-based protocols to maximize success rates. We carefully evaluate each patient to determine if spinal cord stimulation is appropriate for their specific condition.
How much does post-laminectomy syndrome treatment cost?
Post-laminectomy syndrome treatment costs range from $50-$150 per physical therapy session to $20,000-$50,000 for spinal cord stimulation. Most treatments are covered by insurance, significantly reducing out-of-pocket expenses.
Average treatment costs (without insurance):
Conservative treatments:
- Physical therapy: $50-$150 per session
- Medication management: $100-$500 per month
- Epidural steroid injections: $1,000-$3,000 per injection
- MRI imaging: $500-$3,000
Interventional procedures:
- Nerve blocks: $500-$2,500 per session
- Radiofrequency ablation: $3,000-$8,000 per procedure
- Spinal cord stimulation trial: $5,000-$10,000
- Permanent SCS implant: $20,000-$50,000 (total)
- Revision surgery: $30,000-$80,000
Insurance coverage typically reduces costs by 70-90% for medically necessary treatments. Most major insurance plans cover post-laminectomy syndrome treatment when conservative options are tried first.
At Verispine Joint Centers, our billing specialists provide detailed cost estimates based on your specific treatment plan and insurance coverage. We accept most major insurance plans and offer payment options. Call 678-782-7999 to discuss your specific costs and coverage.
Does insurance cover failed back surgery syndrome treatment?
Yes, most major insurance plans cover failed back surgery syndrome treatment, including Medicare and Medicaid. Coverage typically includes conservative treatments, diagnostic procedures, and interventional therapies when medically necessary.
Commonly covered treatments:
Usually covered without pre-authorization:
- Physical therapy (typically 12-20 sessions)
- Medication management and pain medications
- Diagnostic imaging (MRI, CT scans, X-rays)
- Office visits and consultations
- Blood tests and EMG testing
Covered with medical necessity documentation:
- Epidural steroid injections (3-6 per year)
- Nerve blocks and diagnostic injections
- Radiofrequency ablation procedures
- Spinal cord stimulation (after conservative treatment fails)
Insurance requirements for coverage:
- Documentation of failed conservative treatment (typically 3-6 months)
- Medical necessity justification from your physician
- Pre-authorization for advanced procedures
- Step-care approach (trying conservative options first)
Coverage rates by insurance type:
- Commercial insurance: 80-100% coverage after deductible
- Medicare: 80% coverage after Part B deductible
- Medicaid: Varies by state, typically 80-100%
- Workers’ compensation: Usually 100% coverage
Spinal cord stimulation requires pre-authorization and documentation that conservative treatments have been unsuccessful. Most insurers follow Medicare guidelines, requiring at least 3-6 months of documented conservative treatment before approving advanced interventions.
At Verispine Joint Centers, our insurance specialists handle authorization and work directly with your insurance company to maximize benefits. We accept most major insurance plans. Call 678-782-7999 to verify your coverage before your appointment.
Schedule Your Post-Laminectomy Syndrome Consultation in Atlanta
Let Verispine Joint Centers Help You
At Verispine Joint Centers, we understand the challenges of living with post-laminectomy syndrome and are dedicated to helping you find relief from chronic pain. Our team of experienced spine specialists, pain physicians, and therapists works together to create personalized treatment plans tailored to your specific needs.
If you’re struggling with persistent pain after spinal surgery, don’t wait to seek help.
Contact us today at 678-782-7999 to schedule a consultation and take the first step toward a pain-free life. Let us help you regain control and improve your quality of life.