Spinal Stenosis | Understanding the Condition and Finding Relief
Spinal stenosis is a common condition that occurs when the spaces within the spine become too narrow, putting pressure on the spinal cord and nerve roots. This narrowing can lead to pain, numbness, weakness, and reduced mobility, especially in the lower back or neck.
Whether caused by aging, injury, or degenerative changes in the spinal column, spinal stenosis can significantly affect daily life. With early diagnosis and the right treatment, many people find lasting relief and improved function without surgery.
What Is Spinal Stenosis?
Spinal stenosis is a condition where the spaces within the spine become narrow, placing pressure on the spinal cord and nerve roots.
Narrowing of the Spinal Canal
Spinal stenosis occurs when the spinal canal becomes too tight. The spinal canal protects the spinal cord and nerves. When this space shrinks, it can compress nerve roots and interfere with how signals travel through the nervous system.
This narrowing can affect different parts of the spine, including the lumbar spine, thoracic spine, or cervical spine. Lumbar spinal stenosis is the most common form and often causes back pain, leg pain, and trouble walking.
Pressure on Spinal Nerves
As the spinal canal narrows, pressure builds around the spinal nerves. This compression can lead to numbness or tingling, burning pain, and muscle weakness. Some people experience neurogenic claudication, which causes pain in the legs while standing or walking that improves when sitting or bending forward.
The pressure can also affect bladder function, sexual function, and overall mobility in severe cases.
Causes of Spinal Stenosis
The most common cause is degenerative changes from aging. Over time, bone spurs, herniated disks, thickened ligaments, and wear in the facet joints can lead to a narrow spinal canal. Other causes include spinal dysraphism, trauma, or bone conditions like Paget’s disease.
These structural changes reduce space in the spine and affect how the nerve roots exit the spinal column.
Spinal Stenosis Can Develop Slowly
Spinal stenosis may take years to develop. Many people do not notice symptoms until the pressure on the spinal cord or nerves becomes more severe. Once symptoms appear, they may slowly worsen, especially without treatment.
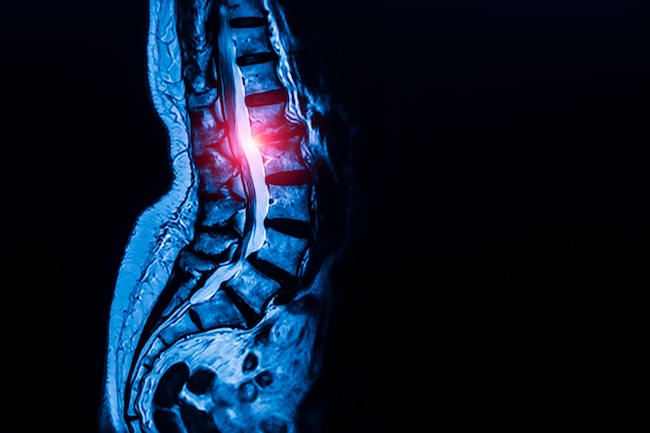
Early diagnosis through a physical exam, review of medical history, and imaging like magnetic resonance imaging (MRI) helps identify the cause and guide treatment.
Common Causes of Spinal Stenosis
Spinal stenosis can result from several structural changes in the spine that place pressure on the spinal cord and nerve roots.
Degenerative Changes in the Spine
Aging is the leading cause of spinal stenosis. Over time, degenerative disorders affect the spinal column, especially in the lumbar spine and cervical spine. The facet joints may become enlarged, and the intervertebral disks can wear down. These changes reduce the space in the spinal canal and increase stress on the nerve roots.
Bone spurs may also develop as the body responds to joint damage. These growths can push into the spinal canal and contribute to nerve compression.
Herniated Disks and Thickened Ligaments
A herniated disk occurs when the soft center of a disk pushes through a crack in the outer layer. This material can press against spinal nerves, causing pain and weakness.
As the spine ages, ligaments that support it can become thickened and less flexible. These stiff ligaments may bulge into the spinal canal and reduce available space, further narrowing the passage for the spinal cord and nerves.
Spinal Injuries and Instability
Trauma from falls, car accidents, or direct impact can displace spinal bones or damage surrounding soft tissue. These injuries may cause swelling or lead to spinal instability, increasing the risk of stenosis.
Fractures and misaligned vertebrae can interfere with how nerve roots exit the spinal canal. In some cases, previous back surgery can also lead to scar tissue that contributes to narrowing.
Bone Conditions and Structural Disorders
Certain bone diseases like Paget’s disease can change the bone structure and enlarge vertebrae, crowding the spinal canal. Genetic conditions such as spinal dysraphism can also result in a smaller-than-normal canal from birth.
These disorders may affect both the thoracic and lumbar spine, leading to early symptoms and limiting flexibility and function.
Other Contributing Factors
Less common causes include tumors, cysts, or abnormal growths that develop in or around the spine. These may press on nerves and restrict the space available in the spinal canal. Inflammation from infection or autoimmune conditions can also contribute to narrowing.
Understanding the cause of spinal stenosis is key to choosing the right treatment and working to relieve symptoms and prevent worsening.
Recognizing Spinal Stenosis Symptoms
Spinal stenosis symptoms vary depending on the location and severity of spinal canal narrowing. These symptoms often develop gradually and may worsen over time.
Pain in the Back, Neck, or Legs
Back pain is a common sign of lumbar spinal stenosis. It may be sharp or dull and can spread to the hips or legs. When the cervical spine is affected, people may feel neck pain and stiffness. Pain often increases with walking or standing and improves when sitting or leaning forward.
Leg pain linked to neurogenic claudication may cause cramping or weakness, especially during physical activity. Rest usually helps relieve this discomfort.
Numbness, Tingling, and Weakness
Narrowing of the spinal canal can compress the nerve roots, leading to numbness or tingling in the arms, hands, legs, or feet. The sensation may feel like burning or electric shocks. Over time, muscle weakness may affect walking or balance.
Some people develop foot drop, where the front of the foot drags while walking due to reduced nerve control.
Loss of Bladder or Sexual Function
Severe nerve compression can interfere with bladder function or sexual function. These symptoms may include incontinence, reduced sensation, or difficulty with control. These signs often indicate serious pressure on the spinal cord and need immediate medical attention.
Fluctuating or Worsening Symptoms
Spinal stenosis symptoms often develop slowly. Some people experience mild discomfort that comes and goes, while others notice steady worsening. As the spinal nerves remain under pressure, symptoms can become more frequent and disruptive. Early recognition can lead to faster treatment and better long-term outcomes.
Diagnostic Process: Precision is Power
Accurate diagnosis is essential for identifying spinal stenosis and developing an effective treatment plan. Clear evaluation helps confirm the cause of symptoms and the extent of spinal canal narrowing.
Reviewing Medical History
The diagnostic process starts with a full review of medical history. This includes past injuries, prior back surgery, and long-term conditions that affect the spinal column. Details about pain patterns, numbness or tingling, and changes in bladder function help identify possible nerve involvement.
A history of degenerative disorders or bone conditions like Paget’s disease may increase the risk of spinal stenosis.
Physical Exam
A focused physical exam follows the history review. The provider checks posture, range of motion, muscle strength, and reflexes. Signs of foot drop, muscle weakness, or reduced sensation can signal nerve compression. Walking tests may be used to evaluate neurogenic claudication and leg strength under pressure.
Pain that improves when patients bend forward or lean forward often points to lumbar spinal stenosis.
Imaging Tests
Imaging is used to confirm the diagnosis and view the structure of the spinal canal. Magnetic resonance imaging (MRI) is the most common test. It shows soft tissue, spinal nerves, and any herniated disk or thickened ligaments.
Computed tomography (CT) scans may be used with contrast dye to provide a detailed view of the bone structure and detect bone spurs or narrowed areas. These scans help identify exactly where spinal stenosis occurs.
Role of Imaging in Planning Treatment
Imaging helps define the severity and location of the stenosis. This guides decisions on physical therapy, anti-inflammatory medications, or spine surgery. It also shows if there is spinal instability that may require spinal fusion or other interventions.
Each part of the diagnostic process supports a focused approach to relieve pressure and restore function.
Non-Surgical Treatments for Spinal Stenosis
Many people with spinal stenosis find relief through non-surgical treatments. These options help reduce pain, improve mobility, and slow the progression of symptoms.
Physical Therapy
Physical therapy strengthens the muscles that support the spinal column and improves flexibility. A physical therapist may guide exercises that reduce pressure on the spinal nerves and improve posture. Movement and strength in the back muscles, hips, and legs can help relieve symptoms.
Therapy often focuses on positions that reduce discomfort, such as bending forward or leaning forward. These movements open the spinal canal and reduce nerve compression.
Anti-Inflammatory Medications
Non-steroidal anti-inflammatory drugs (NSAIDs) are commonly used to manage spinal stenosis symptoms. These medications reduce swelling and help relieve pain caused by nerve compression or irritated tissue. Some people may also benefit from short-term use of muscle relaxants or nerve pain medications.
Anti-inflammatory medications are often combined with other treatments for better results.
Activity Modifications
Daily habits can affect how much pressure is placed on the spine. Patients are often advised to avoid prolonged standing or walking on hard surfaces. Adjusting how one sits, lifts, or moves can reduce strain on the lumbar spine and thoracic spine.
Simple changes, such as using support cushions or avoiding twisting motions, may reduce irritation of the facet joints and nerve roots.
Alternative Therapies
Some people with spinal stenosis use alternative therapies such as acupuncture, chiropractic care, or massage. These methods may help reduce tension and improve circulation in the surrounding soft tissue. While results vary, they may provide temporary pain relief in combination with medical care.
All therapy choices should be discussed with a specialist to avoid worsening symptoms.
Epidural Injections
In some cases, corticosteroid injections are used to reduce inflammation around the spinal cord or nerve roots. These injections target areas of swelling and may offer short-term relief. They do not correct the narrowing but may allow for better mobility and participation in physical therapy.
Non-surgical treatment works best when combined with early diagnosis and consistent follow-up. It is often the first step before considering more advanced interventions.
Life After Diagnosis: Living With Spinal Stenosis
Managing spinal stenosis is an ongoing process. With the right plan, many people can reduce symptoms and maintain function over time.
Managing Daily Activities
People with spinal stenosis often need to adjust how they move and rest. Activities that place stress on the lumbar spine or thoracic spine should be limited. Sitting in a forward-leaning position may relieve pressure on the spinal cord and nerve roots. Walking with support or using assistive devices can also help.
Planning rest periods throughout the day prevents overuse and allows the back muscles to recover.
Staying Active and Strong
Regular, low-impact exercise supports the spine. Walking, swimming, or cycling can improve blood flow and reduce stiffness. Physical therapy may continue after diagnosis to help with stretching, posture, and balance. Strengthening nearby muscles helps reduce strain on the facet joints and spinal column.
A physical therapist can recommend exercises based on the type and severity of spinal stenosis symptoms.
Watching for Worsening Symptoms
Even with good habits, spinal stenosis symptoms can change. New numbness or tingling, increased leg pain, or signs of foot drop should be reported quickly. Loss of bladder function or severe weakness may mean greater nerve compression. These symptoms may require updated imaging or a change in treatment.
Routine checkups help monitor progress and adjust the care plan.
Long-Term Outlook
Living with spinal stenosis often means finding the right balance between rest and activity. With early treatment and good self-care, many people avoid surgery. In more serious cases, surgery may be needed to restore function and reduce pressure on the spinal nerves.
The body may respond well over time, especially with support from trained specialists. Ongoing care helps reduce flare-ups and keeps symptoms manageable.
Why Choose Verispine Joint Centers
Choosing the right care team for spinal stenosis is important. Verispine Joint Centers focuses on accurate diagnosis, advanced treatment, and long-term results.
Focus on Precision and Outcomes
Verispine uses proven diagnostic tools, including magnetic resonance imaging (MRI) and computed tomography, to locate areas of nerve compression, spinal instability, or narrow spinal canal. Each patient receives a detailed evaluation that includes a review of medical history, a complete physical exam, and targeted imaging.
Clear diagnosis leads to better care and better outcomes.
Expertise in Non-Surgical and Surgical Care
Verispine offers both non-surgical treatment and surgical options. Many patients begin with physical therapy, anti-inflammatory medications, and lifestyle changes to help relieve symptoms and improve movement. If needed, advanced procedures such as spinal fusion or decompression may be recommended.
Every treatment plan is based on what works best for the individual’s condition and goals.
A Team Built Around the Patient
The Verispine team includes skilled orthopedic surgeons, pain specialists, and physical medicine providers. Each specialist works together to manage pain, improve function, and restore quality of life. The care team guides patients through each step with clear instructions and consistent follow-up.
This support helps people with spinal stenosis make steady progress with fewer setbacks.
Multiple Locations
Verispine Joint Centers has multiple locations, including Stockbridge, Hapeville, Roswell, Decatur, and Lawrenceville. This allows more patients to receive expert spine care without delay.
Access to high-quality care close to home makes it easier to manage spinal stenosis over time.
Take the Next Step Toward Relief With Verispine Joint Centers!
If you’re living with symptoms of spinal stenosis, you don’t have to manage them alone. The team at Verispine Joint Centers is here to help you find answers and build a treatment plan that fits your needs.
From precise diagnosis to advanced care, our specialists focus on relieving pressure, restoring function, and helping you move with confidence again. Schedule a consultation today at 678-782-7999 at one of our locations and take the first step toward lasting relief.